Campylobacteriosis is a bacterial infection caused by a bacterium called Campylobacter bacteria (mostly C. jejuni). Among the most common bacterial infections among humans, it is more often a foodborne illness. This bacterium sometimes causes abortion in the animals and food poisoning in the humans.
Similar to a disease called salmonella infection, campylobacteriosis can be caused by eating uncooked poultry. It can lead to cramps, fever, inflammatory diarrhea (sometimes bloody) or dysentery syndrome and sometimes other serious complications.
The infants and children are at a higher risk of having the infection than the adults but it can occur at any age. Also, the males have more chances of getting infected than females. The infection is more common in summer than winter.
Here’s a quick look at the causes, signs & symptoms, diagnosis, treatment and preventions of campylobacteriosis.
Risk Factors, Causes & Transmission
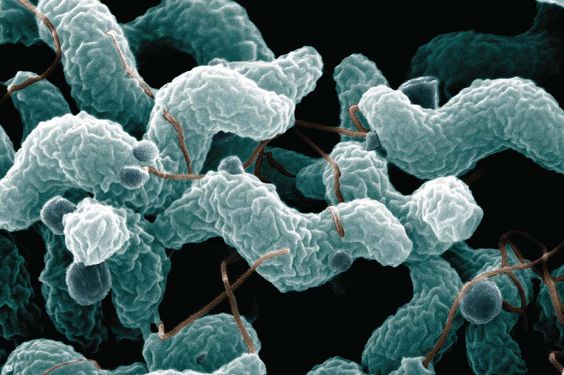
Campylobacter bacteria is responsible for causing campylobacteriosis. In most cases, C. jejuni that is usually found in the cattle, birds and swine is the cause of the illness. But the disease can also result from C. coli (swine, birds and cattle), C. upsaliensis (cats and dogs) and C. lari (seabirds).
The common routes of transmission for the disease-causing bacteria include waterborne (contaminated drinking water and sewage systems), fecal-oral, person-to-person contact, ingestion of contaminated food (usually undercooked or poorly handled poultry and unpasteurized milk) and contact with contaminated livestock & household pets.
Moreover, the animals farmed for meat are the major sources of campylobacteriosis. The wild animal and environmental sources were responsible for just 3% of the disease. The infectious dose is around 1,000 to 10,000 bacteria but even 10-500 bacteria are enough to infect the humans.
The bacterial exposure is often more common at the time of traveling and thus it is a common type of travelers' diarrhea. Also, it generally develops in isolated cases. Sometimes, though, an outbreak can occur when many people have the same infection.
Signs & Symptoms

The infection of campylobacteriosis lasts for nearly one week. The infection lasts for nearly one week. If you have ever been infected, the symptoms begin within 1-5 days of consumption of bacteria.
The most common sign of campylobacteriosis is diarrhea (invasive/inflammatory diarrhea). The other signs of infection are:
- Fever
- Abdominal pain and cramps
- Bloating
- Dysentery
- Vomiting
- Myalgia
- Headache
- Frequent bloody bowel movements
These symptoms may be severe lasting for about 24 hours. Also, some people never experience any kind of symptoms. In case of weakened immune system, the illness-causing bacteria can lead to a very serious infection of the bloodstream.
It is classified as invasive/inflammatory diarrhea, also described as bloody diarrhea or dysentery. An effect of this illness is tissue injury in the gut (jejunum, the ileum, and the colon).
Complications
The complications of the disease include prolonged diarrhea, megacolon, sepsis, severe pain in gut or rectum, very high fever and dehydration. They are usually seen in young children and immunocompromised people. A chronic form of disease may develop without a distinct acute phase. The chronic campylobacteriosis is characterized by a long period of subfebrile temperature. Also, asthenia, eye damage, arthritis, endocarditis may develop if the infection is left untreated.
In case of a weakened immune system (due to cancer, HIV or cancer medications), visit a doctor soon after the diarrhea and other symptoms may appear. Infrequent deaths may occur in the young individuals due to blood volume depletion (result of dehydration) and in elderly or immunocompromised people.
In HIV affected patients, the infections may be frequent and it may lead to prolonged bouts of dirty brown diarrhea. This is more commonly associated with bacteremia and antibiotic resistance.
The bacteria may also cause a latent autoimmune effect and damaging effect on the nerves (joining spine and brain to rest of the body) of the legs. It is usually seen many weeks after abdominal surgery. And this effect is known as an acute idiopathic demyelinating polyneuropathy (AIDP) Guillain–Barré syndrome in which an individual experiences ascending paralysis, dysesthesias usually below the waist and respiratory failure in later stages.
In rare cases, this infection may be related to hemolytic uremic syndrome and thrombotic thrombocytopenic purpura.
Diagnosis & Tests
The symptoms of campylobacteriosis such as diarrhea, bloody stools and vomiting may also be the symptoms of several other diseases. For a proper diagnosis, the campylobacter bacteria can be detected by carrying out a Grain stain of a stool sample (with high specificity and sensitivity of nearly 60%) in a laboratory but most often by stool culture.
It may take many days for the result to come. In rare cases, a doctor may order a blood test, but their results take even longer to come, up to 2 weeks.
In the test, the fecal leukocytes should be present and this should indicate the inflammatory nature of the diarrhea. The methods are being developed for detecting the presence of campylobacter organisms such as antigen testing via an EIA or PCR.
Treatment

The campylobacter species show sensitivity toward hydrochloric acid in the stomach. Also, acid reduction treatment can help in reducing the amount of inoculum needed for causing the disease.
The infection is typically self-limiting and mostly, the symptomatic treatment by liquid and electrolyte replacement sufficient for human infections. Most of the people recover from the infection without any medicine or special treatments. Consider drinking lot of fluids in the case of diarrhea. Your doctor may prescribe you medicine to fight the bacterial infection in case of weak immune system.
The antibiotic treatment has a slight effect on the duration of symptoms. Its use isn’t recommended except in high-risk patients having clinical complications. Tetracycline can be used in adults and erythromycin in the children. Some studies suggest that erythromycin helps in quickly eliminating Campylobacter from the stool without affecting the duration of illness. As a result, children experiencing dysentery because of C. jejuni do experience benefits from the early treatment of erythromycin.
So the effect of antibiotic treatment depends on the severity of symptoms. Quinolones are effective if the organism is sensitive. But the high rates of quinolone use in livestock makes quinolones are highly ineffective. The poultry infections were earlier often treated by mass administration of enrofloxacin and sarafloxacin for single instances of infection. It was banned later by FDA as it promoted the development of fluoroquinolone-resistant populations. Ciprofloxacin is a primary broad-spectrum fluoroquinolone used in humans.
The antimotility agents like loperamide can result in long-term illness or intestinal perforation in any invasive diarrhea and thus they should be avoided as much as possible. Moreover, trimethoprim/sulfamethoxazole and ampicillin are not effective against Campylobacter.
The doctors often prescribe levofloxacin at first. But if you cannot take it for some reason,
azithromycin is a common medication that is prescribed. Currently, the growing resistance of Campylobacter to fluoroquinolones and macrolides poses a major concern.
Preventions

The best way of avoiding campylobacteriosis is cooking the poultry to at least 165 degrees F. The meat must be white and not pink. Some other preventive measures recommended by the World Health Organization (WHO) include:
- Washing the hands with soap and clean water before cooking and after touching pet, using toilet, pet feces, poultry or meat.
- Making sure that you or your child with diarrhea wash the hands well.
- Keeping uncooked meat and poultry away from other foods like vegetables. For that, use a separate cutting board, countertops, utensils and cooking surface and clean them well after use.
- Eating only hot-served and cooked food.
- Using only pasteurized dairy products to kill the bacteria.
- Avoiding contact with pet saliva, feces and food.
- Chronating the drinking water to destroy organisms or using a chemical disinfectant.
- Treating with antibiotics may reduce fecal excretion.
- No infected healthcare worker should not provide direct patient care.
- Ensuring that ice is from safe water.
- Washing fruits and vegetables well especially the raw ones. Peel them whenever possible.
- The professional food handlers and people at home should observe hygienic rules of food preparation.
Image Source:
1) pinimg
2) findatopdoc
3) healthtap
4) cdc

