Juvenile idiopathic Arthritis (JIA), also known as juvenile rheumatoid arthritis (JRA), is the most common type of juvenile arthritis. It causes joint inflammation and stiffness for over six weeks in a child who is 16 year old or younger. It usually develops around the age 1-6 but may develop as late as 15 years of age.
JIA is an autoimmune disease: the body mistakenly attacks healthy tissues and cells identifying them as foreign. This non-infective and inflammatory condition has no defined cause. It may be short-term and self-limited or chronic.
Here are the different subtypes, cause, symptoms, complications, diagnosis and treatment of JIA.
Six Subtypes Of Juvenile Idiopathic Arthritis

JIA has six subtypes that are:
1. Oligoarticular JIA or Pauciarticular JRA
Oligoarticular or pauciarticular juvenile arthritis (‘oligo’ and ‘pauci’ mean ‘few’) is a form of arthritis that occurs in four or fewer joints, mostly large joints that include knees, elbows and ankles. The children who are affected by this condition are at a higher risk of getting uveitis (chronic eye inflammation) than children with other subtypes. The children testing positive for antinuclear antibody (ANA) are at the highest risk of developing eye inflammation.
2. Systemic JIA (Still’s disease)
The systemic juvenile idiopathic arthritis leads to inflammation in one or more joints accompanied by high fever and a skin rash. It is sometimes called adolescent onset still’s disease to distinguish it from adult onset still’s disease.
3. Polyarticular JIA (Juvenile RA)
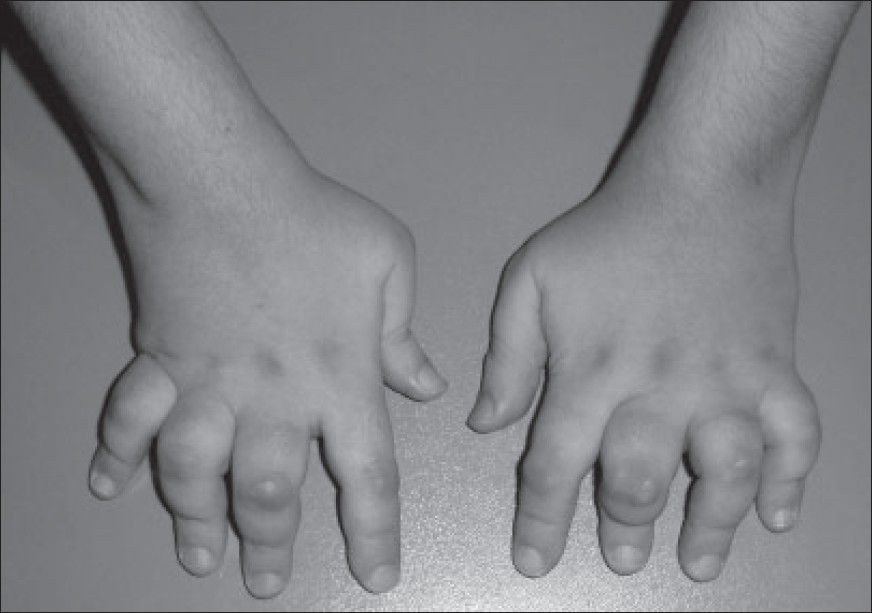
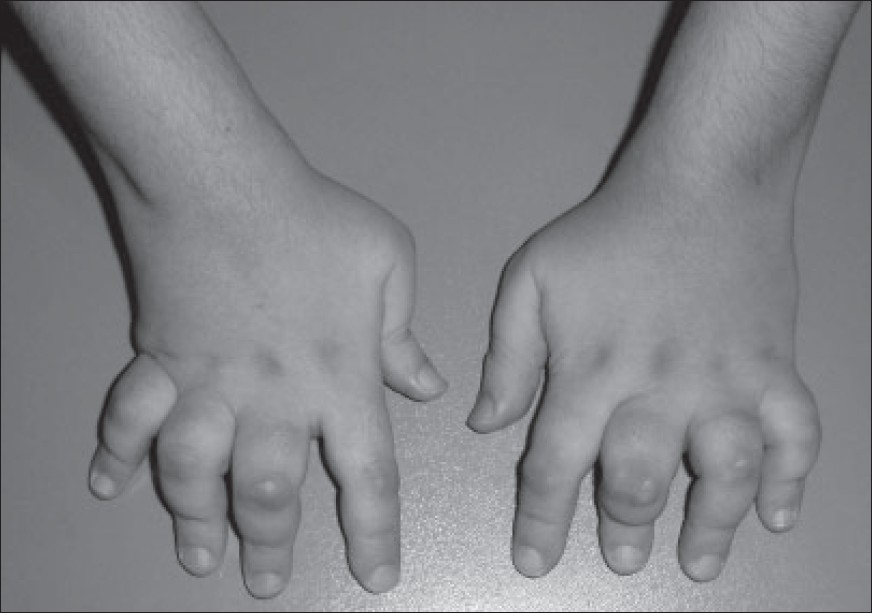
Polyarticular JIA, also called juvenile rheumatoid arthritis, causes inflammation in five or more joints but weight-bearing joints and jaw can also be afflicted. Polyarthritis can either have positive or negative rheumatoid factor.
4. Enthesitis-related JIA
Enthesitis-related arthritis is often referred to as spondyloarthritis an is more common in boys. This condition is described by tenderness where the bone meets a ligament, tendon or connective tissue accompanied by joint inflammation of arthritis. It usually affects knees, hips and feet.
Enthesitis-related arthritis may also involve inflammation in the body parts other than joints. Its onset is around the ages 8-15. The children affected by this condition will often test positive for HLA-B27 gene.
5. Juvenile psoriatic arthritis
Psoriatic arthritis when combines with skin disorder psoriasis leads to a condition in children is known as psoriatic arthritis. The psoriasis may occur several years before joint symptoms appear. The joint symptoms pain and swelling in one or more joints usually the wrists, knees, ankles, fingers and toes. The symptoms of psoriasis include a scaling red rash commonly seen behind the ears; on the eyelids, elbows and knees; at the scalp line; or in the belly button.
6. Undifferentiated JIA
This describes a juvenile arthritis that does not belong to any of the above subtypes and involves symptoms of two or more subtypes.
Cause
The exact cause of juvenile idiopathic arthritis remains unknown (that’s why it is called idiopathic). As some researchers believe, the body tissues and cells are attacked and destroyed by immune system because of genetic and environmental factors. They suggest that certain gene mutations may make a person more vulnerable to environmental factors such as viruses and bacteria, thereby triggering the disease.
Signs & Symptoms
The most common signs and symptoms of JIA include:
-
Swelling: Joint swelling is a very common symptom but is often noticed in larger joints like knee.
-
Pain: While your child might not tell you of the pain, you may notice the limps mainly early morning or after a nap.
-
Rash, fever and swollen lymph nodes: They may occur on the trunk and typically worsen in the evenings.
-
Stiffness: You might notice clumsiness in your child, especially in the morning or after naps.
Complications Of JIA
The various serious complications that may occur from JIA include:
-
Eye problems: Certain forms of juvenile idiopathic arthritis can cause eye inflammation (uveitis). If this condition is not treated, it may lead to cataracts, glaucoma and even blindness. The eye inflammation usually takes place without any symptoms; so it is important that children having this condition are examined by an ophthalmologist on a regular basis.
-
Growth problems: Juvenile idiopathic arthritis can hamper the growth of child growth and his/her bone development. Some of the meds used for treatment especially corticosteroids can also discourage growth.
Diagnosis

These blood tests are carried out for diagnosing juvenile idiopathic arthritis.
-
Rheumatoid factor is the antibody sometimes found in the blood of children who are affected by juvenile idiopathic arthritis.
-
C-reactive protein helps in measuring the levels of general inflammation in the body.
-
Erythrocyte sedimentation rate (ESR) is the speed at which your RBCs settle at the bottom of a tube. A high rate can suggest inflammation. It is mainly used for determining the degree of inflammation.
-
Cyclic citrullinated peptide (CCP) is another antibody that is found in the blood of children who have this condition.
-
Anti-nuclear antibodies are the proteins usually produced by the immune systems of people with certain autoimmune diseases, including arthritis. They are a sign of an increased chance of eye inflammation.
Apart from the blood tests, the imaging scans such as MRI or X-rays may be carried out in order to rule out other conditions (fractures, tumors, infection or congenital defects). They may also be used from time to time after the diagnosis for monitoring bone development and detecting any kind of joint damage.
Treatment

A pediatric rheumatologist who is known to have specialization in treating children with arthritis and other joint problems should be consulted. You can also consult a pediatrician and a rheumatologist. Physical therapists, occupational therapists and rehabilitation specialists called physiatrists can also provide help.
Follow the treatment plan recommended by doctor for easing swelling, maintaining full movement in the affected joints, relieving pain, and preventing/treating complications. Medications and physical therapy prove effective in providing relief.
The medications that are commonly prescribed include:
- NSAIDs or Nonsteroidal anti-inflammatory drugs
These drugs include ibuprofen and naproxen and other prescription drugs. Aspirin is generally not used to treat children but for if given in correct dose, it can control JIA symptoms causing only few side effects.
- Disease-modifying anti-rheumatic drugs (DMARDs)
They are often used if NSAIDs don't seem to work and also prevent the condition from becoming worse. They’re often taken with an NSAID as they take months or weeks to relieve the symptoms.
- Corticosteroids
These meds especially prednisone helps children in stopping severe JRA symptoms like inflammation of the lining around the heart (pericarditis).
- Biologic drugs
They can be effective when other drugs don't work. The doctors might prescribe them on their own or along with other medicines.
Physical therapy is important in keeping the children’s muscles strong so that their joints can move without pain or much effort. A physiatrist or a physical therapist can lay out a exercise program. A specialist may also recommend use of splints and other devices for maintaining normal bone and joint growth. Another alternative or complementary treatment is acupuncture.
Image Source:
1) clinicalpainadvisor
2) pediatricneurosciences
3) spineuniverse
4) tiepermanhealth